Home › Forums › South Africa Today Headline News-NOW HOSTED ON LOVING LIFE TV › Helen Joseph doctors speak out – ‘we won’t give up without a fight’
- This topic is empty.
-
AuthorPosts
-
2022-11-15 at 16:42 #382692
 Nat QuinnKeymaster
Nat QuinnKeymasterThe doctors are taking a stand as the ailing Johannesburg hospital – once a world-class facility – faces collapse.
Not in his wildest dreams did *Dr M imagine he would say his hospital should close its doors or stop accepting patients. Never did *Dr O think she’d cancel surgeries because an unmaintained roof has turned theatre floors into soggy swamps. And never did *Dr D imagine she’d advise friends to emigrate if the government were left to manage the National Health Insurance (NHI).
The three doctors, based at Helen Joseph Hospital (HJH), are exhausted and frustrated, but refuse to be beaten down any further. They remain on the frontline of another kind of “pandemic”, they say: it’s a crisis that threatens to collapse public health services in the province, especially at HJH. But they also won’t give up without a fight for a hospital that was at one time a world-class facility, they say.
Over the past few weeks the three have separately contacted Maverick Citizen, raising the alarm that the public must wake up to mismanagement and incompetence that they believe has allowed the hospital to rush to the brink of dysfunction and collapse.
It’s midweek, late at night when Dr M spells out in a series of WhatsApp messages some of the things that have gone wrong at the Johannesburg West facility. She has arrived home after another long shift. She’s missed dinner and rolling blackouts have kicked in – but she carries on messaging because she cannot stay silent as the government punts the line that “everything is okay” – it’s not.

Portable toilets have had to be installed at Helen Joseph Hospital because of water interruptions and outages. (Photo: Supplied) She says that over the past few years already the doctors have been asking for the HVAC (heating, ventilation, air-conditioning) system to be repaired and maintained. It’s not only for the comfort of ill patients, but because a lack of temperature control is potentially dangerous. There is a raised threat of infection, especially in theatres.
“We have to cancel surgeries, or reschedule them because the coolers don’t work properly, and already we are seeing patients returning to the hospital because of sepsis,” she says.
Doctors increasingly had to try to fix problems themselves – buying supplies, mopping floors and using scrubs and medical bins to collect water dripping into the hospital: “Some time ago some of the doctors suggested we club together to get the aircon fixed but management would not allow it. But when we take up our issues with senior management they give us the same old excuse that it’s the responsibility of the Gauteng department of infrastructure and development, not the Gauteng department of health.”
She says it’s a similar situation with ongoing water interruptions and water shortages at the hospital. Already doctors like Dr M are bringing in water daily for himself and some of his patients. As angry and fed-up as he is, it’s still patient welfare that he won’t turn a blind eye to.
‘Hiding problems’
“Helen Joseph management has become obsolete and problems come from the top – from the Gauteng department of health. They are now hiding problems behind city water problems, but the problems are much bigger and there are also other issues that are not related to water.
“We don’t get much feedback as to what the problems are or why funding that is available is not being used to fix what needs fixing and doctors are left to MacGyver everything to keep working,” he says.
Read in Daily Maverick: “Images reveal how water shedding brings disease and indignity to two major Johannesburg hospitals”
The doctor flags other problems and signs of deep rot and mismanagement – perhaps even misappropriation, he says. Doctors are told there is no linen available but the laundry department continues to operate. Doctors are being made to fill out road accident reports even though there is a Road Accident Fund doctor paid to do the job. There are also random repair jobs such as the replacement of unbroken light switches when more urgent problems should take priority.
And there are problems of the autoclaves, used to sterilise surgical and other equipment, not working; equipment and services have not been paid for by the hospital resulting in medicine shortages; access to the PACS (picture archiving and communication system) has been cancelled because subscriptions have not been paid. It means X-rays have to be located and printed out. When they can’t be found, new ones have to be ordered. The hospital has also had to install portable toilets because many indoor toilets no longer function.
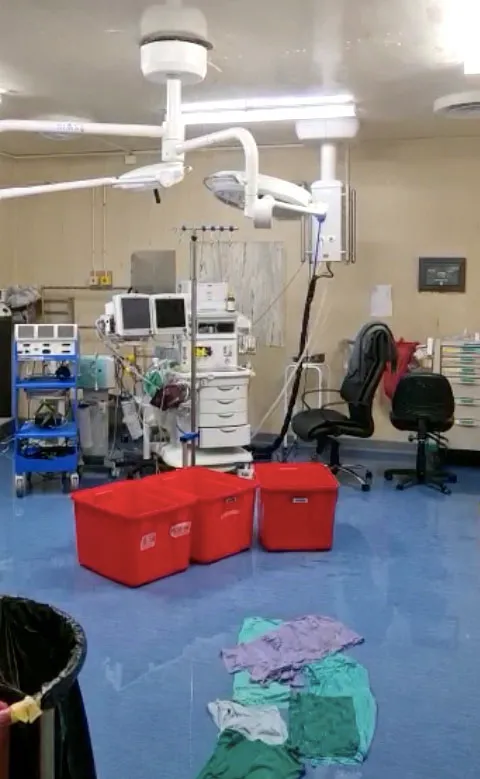
Rain coming through into the theatres at Helen Joseph Hospital. Staff try to catch falling rainwater in containers and use scrubs to mop it up. (Screenshot supplied) “We need to blow the lid off this place. The situation at Helen Joseph should be a national crisis – but this dire issue is just not being discussed. The President has to speak out and have a family meeting to address this issue of our public hospitals,” he says.
Dr D, who finally finds a late Friday afternoon to chat because long days have turned into a long week, describes how a few weeks ago a patient had to remain in theatre after surgery instead of being taken to ICU, because of a shortage of ICU beds. The patient had to be given post-op care in the theatre, creating a bottleneck for surgeries.
“We cannot pretend that everything is fine. I remember a rep said to me that 10 years ago HJH’s theatres were on par with those in the private sector, and now these theatres are putting patients’ lives at risk,” says Dr D.
Read in Daily Maverick: “‘They made her life hell’ – top breast cancer surgeon quits Helen Joseph Hospital, and volunteers follow suit”
Patients are waiting a month for emergency surgeries and elective procedures are constantly postponed, she says.
“Infections can set in and people could lose their limbs or even their lives.”
For Dr D one of the biggest impacts of weakening service delivery at Helen Joseph Hospital is that patients are trusting doctors less and less – even blaming interns when their surgeries are cancelled. She says there are even rumours circulating that patients should bribe doctors to get onto surgery lists.
They face hostility not just from patients but also senior clinical management who, she says, resort to intimidation and bullying as a management style when they deal with consultants.
“It makes you so despondent. If we do our jobs well then we can heal our patients, but we just don’t have the resources or the support from clinical managers and management to do our jobs,” she says.
The doctor adds that weekly departmental reports submitted to clinical managers never receive any acknowledgment, let alone feedback.
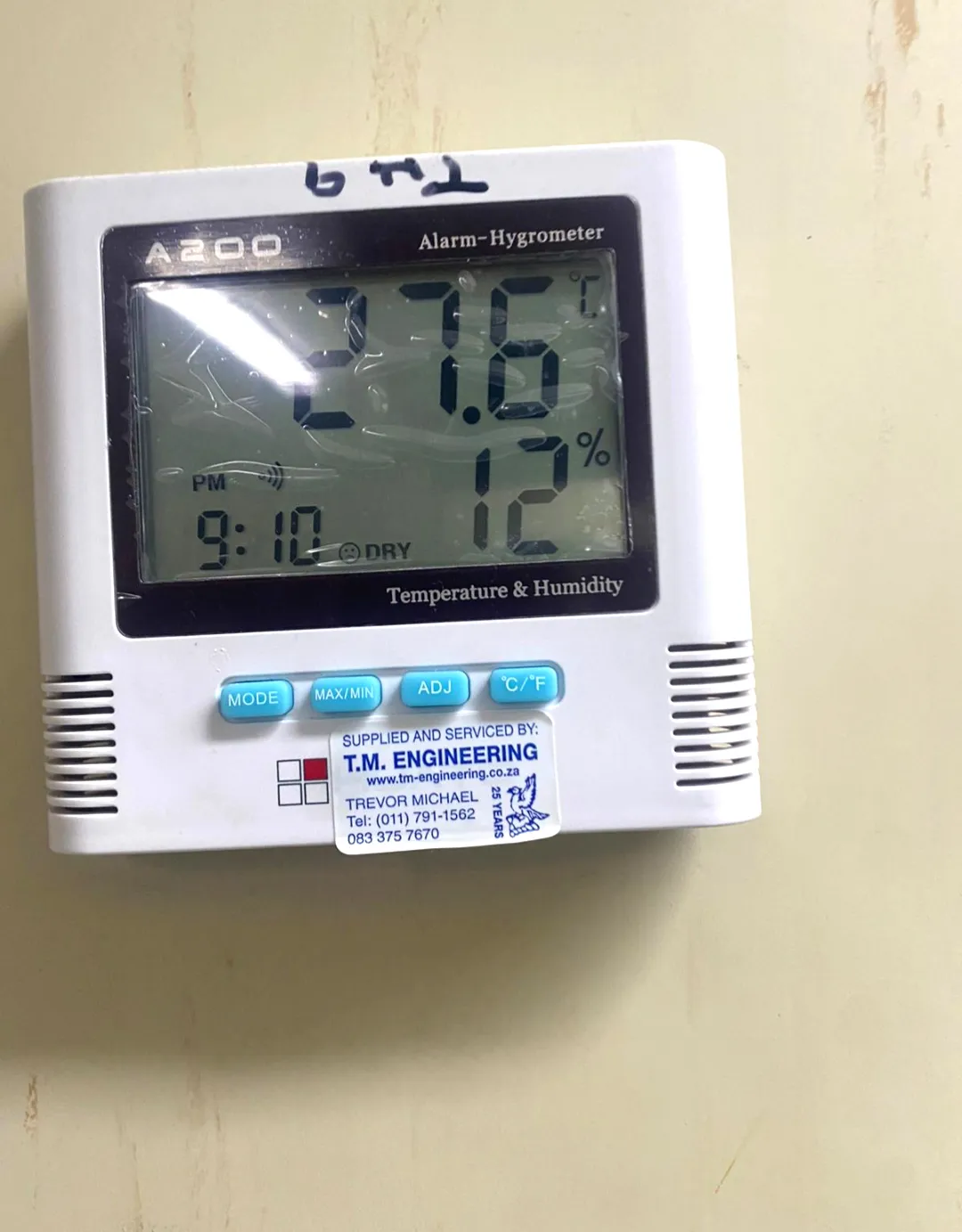
Broken air-conditioning systems mean temperature control is compromised. This picture shows the air-conditioning temperature stuck at a high 27.6°C. (Photo: Supplied) “There was an HOD who was asked how he is going to sort out a maintenance problem in the hospital, but he’s not a doctor – it’s not his role. We also never see the CEO or senior management on the hospital floor, it should be their job, so they get to understand the day-to-day realities we are facing,” she says.
“The doctors are willing to go the extra mile and they are hard-working, but they can’t go on like this forever and it’s not why we trained to be doctors.”
For now, Dr D is determined to carry on fighting and her call is for the public and doctors to lay formal complaints at the hospital.
“I’ve decided to do this even though I have the quality assurance people complaining about it because it’s extra paperwork and they try to scare me off with the extra admin, but I’m not going to stop. I’m also encouraging all the doctors to not leave the public sector and for the public also to make the effort to complain formally because we need to have records of what’s going wrong.
Read in Daily Maverick:
“Charlotte Maxeke closure is placing ‘severe strain’ on Helen Joseph”
“The public must demand better. And we need people who run this hospital to be fit to do the job – not people who have been demoted and moved around from province to province just so they can keep a job. If they can’t do the job they must go.
“I know the doctors don’t feel like they can’t go on much longer; but we must fight on – because our patients are dying.”
Hospital response
CEO of Helen Joseph Hospital Dr Relebohile Ncha responded to Maverick Citizen via Gauteng health department communications. She says the hospital is “not collapsing” but its problems stem from being a 50-year-old building with “ailing infrastructure”, including leaking roofs. Work on the roofs would begin once a contractor was appointed, while work on the HVAC system had already begun.
Ncha calls this a “recent challenge”, but acknowledges that it has delayed operation.
“However, claims that there has been an increase in surgical complications due to suboptimal theatre conditions are inaccurate as the current data does not indicate an increase in that regard.”

Helen Joseph Hospital CEO Dr Relebohile Ncha. (Photo: Julia Evans) As for the hiccups in radiology, she says the PACS system for X-rays is being upgraded but is “waiting for the finalisations from the provincial structures”. She adds: “We are currently printing X-rays for clinicians, therefore no data is lost and no files are lost.”
She also maintains that there is no shortage of ICU beds, as the facility has 14 of these.
On the issue of communication to staff, Ncha says: “The hospital has always been transparent with sharing of information to all staff members. Challenges are discussed at the executive level and decisions are taken and communicated to the staff via their respective managers as well as on a public platform at the hospital.”
But she adds: “It is not procedural to allow staff members to fix items while there are departments that are responsible for fixing those items.”
And while doctors continue to ask for their identities to be protected, Ncha says there is no intimidation or prevention of any staff member from speaking up, but she says matters should be resolved through internal processes. She confirms that there are tensions between clinical managers and consultants but that this “has received attention from the [department] and is being addressed”. DM/MC
* Identities withheld to protect doctors from being targeted for speaking out publicly.
-
AuthorPosts
- You must be logged in to reply to this topic.